
Exoskeletons can augment the performance of unimpaired users and restore movement in individuals with gait impairments. Knowledge of how users interact with wearable devices and of the physiology of locomotion have informed the design of rigid and soft exoskeletons that can specifically target a single joint or a single activity. In this Review, we highlight the main advances of the past two decades in exoskeleton technology and in the development of lower-extremity exoskeletons for locomotor assistance, discuss research needs for such wearable robots and the clinical requirements for exoskeleton-assisted gait rehabilitation, and outline the main clinical challenges and opportunities for exoskeleton technology.



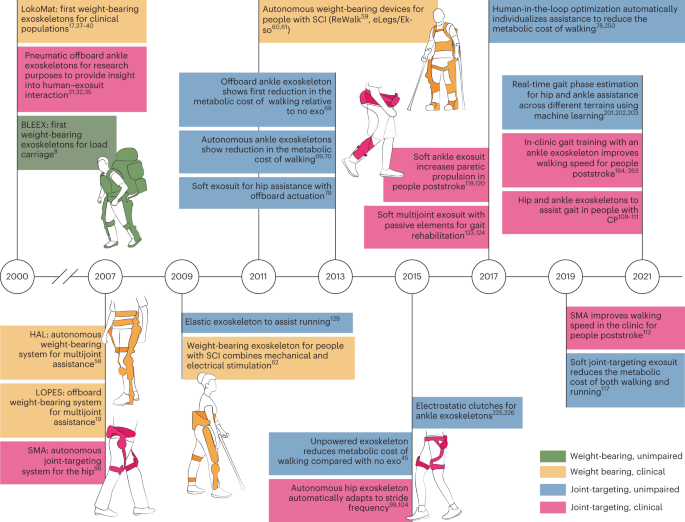
Exoskeletons aiding locomotion entered the popular imagination over a century ago, followed by a series of early patents and prototypes 1,2,3,4,5 . Among other advances in the late twentieth and early twenty-first century, funding from the Exoskeleton for Human Performance Augmentation Program 6 of the Defense Advanced Research Projects Agency (DARPA) of the United States enabled the development of wearable robotic devices for the lower extremities (in particular, the Berkeley lower-extremity exoskeleton, BLEEX 7,8 ; the Sarcos Guardian XO 9 ; and the MIT quasi-passive exoskeleton 10,11,12,13 ) to augment strength and reduce effort during the carriage of load. By taking load off the wearer and providing assistive joint torques during walking, these weight-bearing lower-extremity exoskeletons sought to increase load capacity, improve efficiency and endurance, and reduce the perceived difficulty of walking 11 , potentially benefitting military personnel, first responders and weekend warriors. Measuring the metabolic cost of exoskeleton-aided locomotion became the gold standard for quantifying wearer effort and exertion. As such, demonstrating metabolic cost reductions compared to walking without the robot became a major goal for exoskeletons designed to augment strength and performance. Despite their promise, lower-extremity exoskeletons for performance augmentation in unimpaired users initially failed to demonstrate metabolic cost reductions compared with walking without the exoskeletons 14,15,16 . Therefore, lighter-weight hardware and autonomous systems were developed and tested in goal-driven experiments, with single-joint systems tested to explore underlying biological mechanisms. These technological advances ultimately enabled exoskeletons to meet the envisioned objectives of reducing the metabolic cost during loaded or unloaded locomotion for military, industrial and recreational applications.
Alongside the development of exoskeletons to enhance the performance of load carriage, devices (in particular, the Lokomat 17 , Gait Trainer 18 , lower extremity powered exoskeleton (LOPES) 19 , active leg exoskeleton (ALEX) 20,21 and Rutgers Ankle 22 ) were designed to mechanize physical therapy for individuals re-learning to walk following spinal-cord injury (SCI) or stroke. Common clinical practice calls for physical therapists to manually move the feet and legs of non-ambulatory patients through the motions of walking to facilitate re-learning of movement patterns for functional improvement 23 . Robotic devices were developed to offload this burden from physical therapists and to improve patient outcomes by delivering precise interventions and training at optimal intensities, unconstrained by the limits of manual assistance. Exoskeletons initially failed to show clinical improvements that would justify their cost compared to traditional non-robotic gait-training methods 24,25,26,27,28,29,30 . However, a better understanding of the underlying biomechanics and physiology led to an improvement in exoskeleton design, including biologically inspired strategies for actuation and control 31,32,33,34,35,36 . For example, ‘patient-cooperative control’ has been implemented in devices for gait rehabilitation to allow for more individualized assistance 37,38,39,40,41,42,43 . Such ‘assist as needed’ approaches are particularly important for augmenting the gait of individuals with some residual walking function while encouraging their own contributions.
In this Review, we first synthesize key advances in exoskeleton technology in the early twenty-first century and highlight recent exoskeleton designs, offering clinical insight into how exoskeletons can improve gait rehabilitation and identifying future directions for wearable robots. For devices designed for unimpaired adults, we focus on gait and exclude research in industrial applications (unless they are particularly relevant). We then discuss exoskeletons aimed at reducing the metabolic cost of walking in unimpaired individuals, which has been a principal focus since the 1990s. For devices intended to be used for people with gait impairments, we exclude research reported only in animal models. Rather, we include representative studies of people with stroke, traumatic brain injury (TBI), multiple sclerosis (MS), cerebral palsy (CP), and complete and incomplete spinal-cord injury (SCI-c, SCI-i). These conditions represent a range of gait impairments that require anywhere from full assistance (the case of SCI) to partial assistance (the case of stroke, MS, TBI and CP).
The Cybathlon—a non-profit project of the Swiss Federal Institute of Technology in Zürich, in which people with physical disabilities compete against each other every 4 years to complete everyday tasks using assistive technologies—has showcased a variety of exoskeletons used in various challenges 44 . Lower-extremity exoskeletons are similar to one another in their ability to augment human performance or restore movement; however, they differ in some key characteristics, such as device function and purpose.
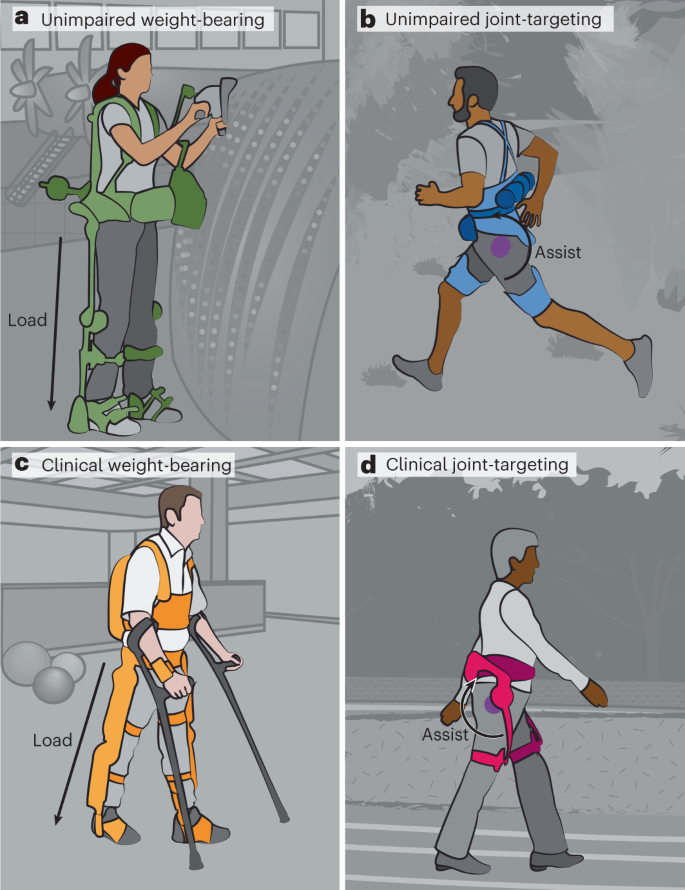
Exoskeletons can be broadly classified as weight-bearing devices that transfer load directly to the ground or as joint-targeting devices that augment biological torque at a specific joint or joints to achieve a physiological goal. Weight-bearing and joint-targeting exoskeletons can either be applied for performance augmentation in unimpaired users or for movement restoration in the clinic for people with disabilities (Fig. 1). These exoskeletons can further be designed with different power sources. Autonomous devices require the user to carry a battery to power conventional actuators (which increases their weight). In research-focused systems, the power source and actuators can be placed on a freestanding offboard structure (tethering the wearer to a treadmill). Alternatively, passive designs, in which energy is collected and returned during the gait cycle, do not require any power source 45 . System-level advances in both exoskeleton types have led to their increased commercial presence, to informative clinical investigations and to a better understanding of how exoskeletons influence biological processes 46,47,48,49,50,51 .
Weight-bearing exoskeletons typically span the entire lower extremity and are made of rigid robotic components that enable multijoint assistance and direct transfer of load to the ground. Such devices were initially designed to reduce metabolic cost in unimpaired individuals during walking. However, to transfer loads to the ground, these devices usually inhibit coordination between the device and the wearer, which causes a change in the wearer’s gait pattern (compared with their optimal pattern), limiting the ability of autonomous weight-bearing devices to lower the metabolic cost of walking 14 . Therefore, weight-bearing exoskeleton technologies have focused on increasing force production during non-ambulatory tasks, for example to enable workers to lift heavy loads for extended periods of time (FORTIS, Guardian XO, Hanyang Exoskeleton Assistive Robot (HEXAR)-CR50 52 , Body Extender 53,54,55 ).
Autonomous weight-bearing exoskeletons can also be designed with high power to restore some degree of mobility in people with substantial walking impairments. Several such devices have achieved regulatory approval 56 (in particular, Hybrid Limb Assist (HAL) 57,58 in Japan and Europe, and ReWalk 59 , EksoNR 60,61 and Indego 62 in the United States). Originally designed to support people with paraplegia, these devices can also be applied as gait-training tools for individuals with residual walking capacity 49 . A variety of such weight-bearing exoskeletons are commercially available (the Atlas, the ExoAtlet, the Hank, the Mina, the SuitX, the ExoH2 and the Twiice).
These devices can further be designed with various features; for example, extended sensor modalities can be integrated in control loops to measure reaction forces between the wearer and the ground 58,63 , the centre-of-mass position 64 , or brain activity 65,66 . Such features may enable the development of weight-bearing exoskeletons with well-coordinated control, allowing the wearer to adapt to new environments with the ease of an unimpaired walker, rather than providing only predefined motions. However, their weight and size limit their capacity to achieve specific physiological goals, such as reducing metabolic cost, because the exoskeleton spans the entire lower extremity and assists multiple joints. Therefore, research efforts have been targeted towards the design of lightweight systems that, instead of transferring load directly to the ground, apply torque in conjunction with biological mechanisms to assist a single joint.
Joint-targeting devices assist a specific part of the body, enabling insights into how distinct biological features respond to changes in targeted exoskeleton assistance, which cannot be achieved with weight-bearing devices. The physiological effects of joint-targeting exoskeletons were first investigated using an ankle system driven by artificial pneumatic muscles 31,32 with an offboard air compressor. By delivering assistance proportional to soleus surface electromyography (EMG), this device not only assisted gait, but also allowed fundamental investigations of the ankle’s function, in particular how passive elements in the ankle muscle–tendon contribute to the efficiency of walking 15,34 . Knowledge gained from these fundamental experiments greatly contributed to the design of joint-targeting devices that can decrease the metabolic cost of walking in unimpaired individuals with powered 67,68,69,70 and passive 45 ankle assistance (Fig. 2). Joint-targeting devices for ankle assistance also contributed to our understanding of gait rehabilitation in people with neurological impairments 71,72,73,74,75 .
Offboard actuation holds an important role in investigating the responses to joint-targeted assistance to inform the design of autonomous exoskeletons. By eliminating the need for body-worn power supplies and actuators, offboard systems enable heavier and more powerful actuators to serve across multiple experiments 76,77,78,79,80,81 , making them ideal research systems for rapid prototyping of joint-targeting exoskeletons. The field of wearable robotics has greatly benefitted from offboard actuation, which has allowed the evaluation of wearer sensitivity to varying levels of augmentation power 82 , the comparison of power-inspired assistance versus moment-inspired assistance 83,84 , the investigation of the impact of the stiffness of elastic ankle exoskeletons, and the optimization of assistance based on real-time measurements of metabolic cost 78,85 . Furthermore, offboard actuation has allowed one device to emulate both rigid-link and non-rigid-link exoskeletons for gait training post-stroke 86 . Additionally, a commercial offboard system (Caplex) can emulate the evaluation of assistive strategies in real time 77 .
The mechanical designs and control strategies of joint-targeting exoskeletons with offboard actuation can be easily modified to explore the different physiological impacts of the designs; however, these systems are restricted to treadmill-based studies, which may not reflect typical features of walking (such as changes in speed, direction or terrain). By contrast, autonomous systems allow the wearer to freely navigate unconstrained environments. The aim of joint-targeting exoskeletons is not to bear weight, hence autonomous devices do not require large rigid structures. However, rigid components are beneficial for efficiently transferring torques to the body; for example, rigid components and a distal actuator at the ankle decrease the metabolic cost of loaded and unloaded walking in unimpaired individuals 69,70,87 . Rigid devices have also been developed for assisting other joints, in particular the hip 88,89,90,91 and the knee 92,93 , and for multijoint assistance 94 (for example, the Cyberlegs project 95 ). Moreover, rigid joint-targeting autonomous exoskeletons have been commercially developed for industrial, recreational and clinical applications, such as the Stride Management Assist (SMA) 96,97,98 and the Gait Enhancing and Motivation System (GEMS) 99,100 . These autonomous bidirectional hip exoskeletons have been used to investigate new control schemes 101,102,103 , the augmentation of performance in unimpaired individuals 104,105,106 , the restoration of gait function in elderly adults 107,108 , improvements in gait and other mobility in people with CP 109,110,111 and clinical effects post-stroke 112,113 .
Joint-targeting exoskeletons often feature creative designs to mitigate the high energetic cost of distal mass; for example, lightweight textile-based components can be applied to interface with the body and minimize kinematic interference. These soft exoskeletons (often called exosuits) sacrifice some efficiency in transmitting power to the user in exchange for light and minimally restrictive systems, which may be more comfortable to wear for prolonged periods compared with traditionally rigid exoskeletons. Soft exosuits can augment metabolic performance 114,115,116,117,118 and enable post-stroke gait assistance at the ankle 119,120,121 . They have been commercialized (one example is the ReStore 122 ). The textile-based Myosuit assists hip and knee extension with a single actuator, as well as hip flexion with a passive spring-like element during sit-to-stand transitions 123 and walking 124 . A soft wearable robotic ankle-foot orthosis with a bidirectional, tendon-driven and distally mounted actuator can assist plantarflexion and dorsiflexion 125 . A textile-based device with a ‘cross-wire’ design can be applied at the hip to induce turning 126 . The XoSoft delivers similar amounts of mechanical power to the ankle and hip as other devices 127 but has not yet been evaluated in the clinic or in terms of metabolic cost reduction in unimpaired individuals.
To further reduce costly distal mass, designs based on biological mechanisms are being explored. The human body compensates for energy cost with passive structures such as tendons connected to active muscles, which can be mimicked in passive devices that rely only on elastic elements to reduce the cost of walking. For example, such passive ankle devices can reduce the metabolic cost of walking 45 or running 128,129,130 . Furthermore, passive devices, which can be worn under clothes 131 , can assist the hip 132 or ankle during walking.
Exoskeletons have begun to confer the wearer some of the long-hypothesized physiological benefits during locomotion. Devices for unimpaired users can reduce the effort of walking and jogging in lab-based and outdoor settings, and devices for gait rehabilitation have led to clinical improvements. Although the aim of devices for gait rehabilitation is to reduce the metabolic cost of walking, their immediate objective is to modify the wearer’s existing gait pattern. Accordingly, clinically relevant metrics and functional outcomes, such as walking speed and spatiotemporal symmetry, are used to evaluate device benefits. Therefore, understanding the wearer’s response to exoskeletons is crucial to enable the design of robust devices, individualized assistance and widespread user acceptance.
The first demonstration of an offboard ankle-assisting exoskeleton lowering the metabolic cost of walking compared to unassisted walking 68 made clear the promise of joint-targeting exoskeletons. Joint-targeting devices can interface with the body through different approaches, and they can be designed with different actuation and control modes to assist a variety of joint motions, rather than just the ankle. The metabolic impact of these devices varies depending on whether the exoskeleton is autonomous or tethered to an offboard actuator, and on whether the effects of the exoskeleton are compared to walking without an exoskeleton (no exoskeleton) or to walking with an exoskeleton but without assistive torque (no assist).
Studying metabolic-cost reduction using offboard systems and comparisons to no assist allow for rapid iteration through experimental designs and through device and controller prototypes. An offboard ankle-assisting exosuit led to a magnitude of assistance delivered during walking that directly influenced metabolic reduction compared with no assist (22.83 ± 3.2%) 82 . Although the highest augmentation torques may achieve the highest metabolic reduction, well-optimized assistance profiles offer further metabolic benefits over fixed control strategies. Human-in-the-loop (HIL) optimization automatically individualizes control parameters to each participant in real time and has been shown to lead to metabolic reductions using offboard devices assisting the hip (17.4 ± 3.2% compared with no exoskeleton) 85 and the ankle (24.3 ± 7.4% compared with no assist) 78 . Further study at the muscle level may provide more information on optimal profiles or device designs for maximizing metabolic reduction 133 .
For unimpaired users, the ultimate goal of autonomous exoskeletons is to reduce the metabolic cost of walking relative to no exoskeleton; that is, these wearable devices should more than offset the additional weight (including that of power sources) carried by the user. Therefore, exoskeletons not only have to provide assistance at the correct time, but also have to be sufficiently light so that their metabolic benefit overcomes the metabolic burden of the added weight. A landmark study of an ankle-targeting autonomous system showed metabolic reduction during loaded walking (8 ± 3%) compared with no exoskeleton 69 . Other autonomous exoskeletons have also led to metabolic reductions relative to no exoskeleton 134 : a passive ankle device (7.2 ± 2.6%) 45 , a hip exoskeleton (GEMS, 17.4 ± 2.9%) 135 , and a soft exosuit for hip assistance during both walking (9.3 ± 2.2%) 117 and running (4.0 ± 1.3%) 117 .
These results highlight the potential of exoskeletons as assistive complements to walking; however, their design, manufacturing and testing remain time-consuming and resource-consuming. In addition, predicting the efficiency of untested devices in metabolic-cost reduction remains challenging. The increase in metabolic cost owing to exoskeleton weight can be accounted for by the augmentation factor (AF), a metric aimed at predicting the metabolic benefit solely on the basis of its mass and power characteristics 69 . The AF is defined as
$$\mathrmwhere p + is the average positive augmentation power, p dis is the net augmentation-power dissipation (p dis = 0 when |p + | ≥ |p − | and p dis = p + + p − when |p + | < |p − |; p − is the average negative-augmentation power), η is the muscle–tendon apparent efficiency 15 , mi are the added device masses on each segment (trunk, thigh, shank and foot) and βi are the device-location factors for each segment based on linear-regression equations 136 . When the AF was first introduced, only two datasets 67,68 , both assisting ankle plantarflexion, were available to estimate muscle–tendon apparent efficiency, η = 0.41, defined as
$$\eta = \frac<<<\mathrmUsing data published since 2014, focusing on studies demonstrating metabolic reductions relative to no assist, we calculated apparent joint efficiencies for ankle plantarflexion (η = 0.47) 68,69,87,137,138,139 and hip extension (η = 0.49) 117,140,141,142 . Some studies looked at devices that assisted multiple joints 14,143,144,145 . However, some studies did not include all information necessary to compute equation (1), hence we made some assumptions about device parameters, such as weight distribution (Supplementary Table 1). Using these updated apparent joint efficiencies, the AF can predict the metabolic impact of exoskeletons (Fig. 3) for specific modes of assistance (Supplementary Table 2). Of note, a key assumption of the AF is that metabolic benefit from external assistance scales linearly with the average amount of positive power delivered by an exoskeleton. Some studies corroborate this assumption, showing, for example, that the condition with the highest augmentation power shows the highest metabolic-cost reduction 82 ; or that two different assistance profiles with similar amounts of augmentation power lead to similar metabolic reductions 84 . By contrast, empirical experiments 78,83,138 and simulations 146,147 have indicated that there is a point at which too much augmentation power may not lead to additional metabolic-cost reductions. Moreover, studies using passive devices have shown the potential for low-positive-power strategies to reduce the metabolic cost of walking 45 .
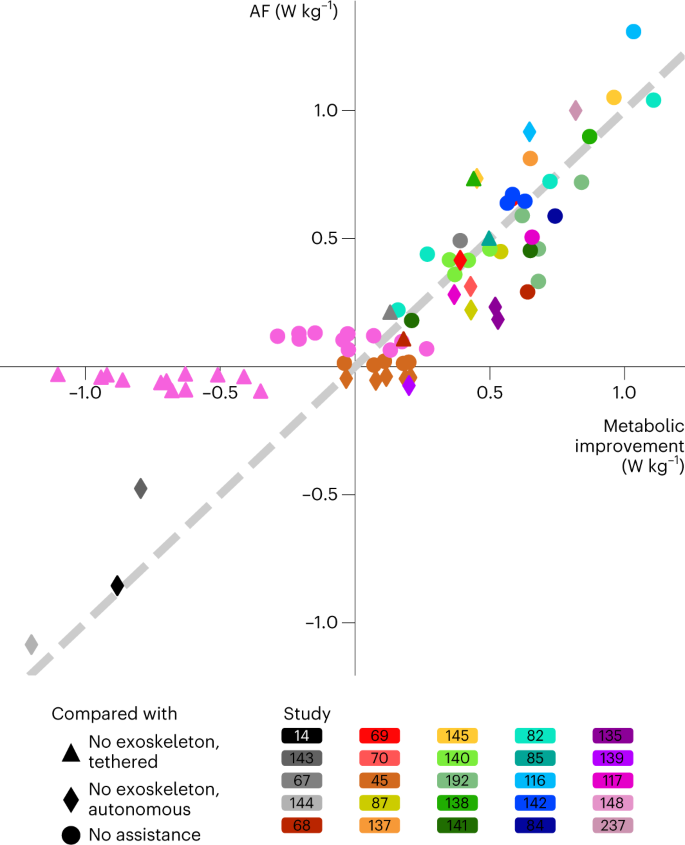
Interestingly, data reported for elastic ankle exoskeletons with intermediate stiffness springs set in parallel with the human plantarflexors do not follow the general trend 148 . This study included actuation profiles that did not provide metabolic improvement; such actuation profiles were also included in another study for unpowered ankle exoskeletons 45 . Actuation profiles that do not decrease the metabolic cost of walking are not common in the recent literature, a gap that perhaps hides factors influencing metabolic benefit. Indeed, augmentation power is not the only factor influencing metabolic improvement. To change the sign of equation (1), the device has to apply substantially more negative augmentation power than positive augmentation power, or needs to be sufficiently heavy so that its distal inertia overrides any benefit of positive augmentation power. In addition, various other factors may influence the metabolic cost.
Device-location factors 136 , for example, do not account for the increased energy cost of moving distal mass at high walking speeds 148 . Moreover, the AF does not consider potentially substantial changes in kinematics owing to exoskeleton assistance 82,148 . Although incomplete, the AF remains a surprisingly powerful indicator of metabolic improvement of devices that apply net positive augmentation power. Studies describing actuation profiles that decrease and increase the metabolic cost of walking will further increase understanding of device designs that make walking easier.
In addition to the AF, other modelling techniques have been used to inform exoskeleton design with the aim of reducing metabolic cost. High-level models such as the individual-limbs method 149 examine how each leg contributes mechanical power to the centre of mass 150 . Interestingly, high-level models have also been used to design a phase-oscillator controller that can reduce the metabolic cost of running compared with no exoskeleton 151 . Future approaches to predicting metabolic-cost reductions should also consider the cost difference in generating force with muscles crossing the hip, knee or ankle. Tools such as OpenSim 152,153,154 can estimate individual muscle activations and kinetics, offering insights into how exoskeletons can modify muscle–tendon dynamics in ways that can either benefit 155 or impede 156 gait.
High-level models can provide information about key trade-offs in the early phases of device development, and more detailed musculoskeletal models can give insight into the biomechanical changes induced by wearable devices. To inform these models, close collaboration between device and simulation designers will be crucial. Experimentalists should provide key experimental data, such as applied device torques and powers, the distribution of added exoskeleton mass on the body, the resultant metabolic impact relative to both no exoskeleton and no assist, and raw kinetic, kinematic or muscle-level responses.
In contrast to devices designed for unimpaired users, improving walking performance in the clinic often does not focus on reducing metabolic cost. People with gait deficiencies develop atypical movement patterns that are thought to be necessary for stability, and devices applied to improve gait may therefore disrupt energetic efficiencies established through these compensations. Although metabolic cost remains important, clinical studies involving exoskeletons for gait assistance often focus on safety metrics to establish patient–device agreement, as well as on efficacy metrics based on walking function and quality. Here we discuss outcomes from exoskeleton evaluations in clinical populations ranging from case studies to randomized controlled trials (RCTs).
Weight-bearing exoskeletons have been studied in a range of conditions (from complete SCI to stroke) requiring full to partial assistance, whereas joint-targeting exoskeletons have mainly been used in conditions requiring partial assistance, such as stroke (Table 1). Only preliminary studies have been performed for assessing acceptability and feasibility of wearable exoskeletons in people with SCI thus far, owing to the complex nature of assisting gait in this condition. In clinical studies, exoskeletons have mainly been applied to increase training intensities to facilitate neuroplastic changes, as shown in animal models 157 ; however, certain conditions, such as complete paralysis from SCI, benefit from exoskeletons as an alternative means of mobility.
Table 1 Clinical trials in the past 7 yearsSeveral commercial devices have been examined for their clinical potential, including Ekso 158,159,160 and Indego 161 for SCI, ReWalk for MS 162 , as well as HAL 163 and ReStore 122,164 for stroke. The results have shown acceptable feasibility and safety; however, occurrences of non-injurious falls 158 and skin issues owing to device fit (such as redness and minor abrasion) 122,161 were noted. Although assessments of device efficacy were limited in these preliminary studies, speed-based outcomes improved over the course of robotic gait training in the case of HAL for people with subacute stroke 163 , Ekso for people with SCI 160 and ReWalk for people with MS 162 . In a multisession case study involving three participants with complete SCI, training with the Ekso resulted in linear increases in the number of steps and distances in 2 out of 3 participants, and a 2–3-fold increase in walking speed for all participants 165 . Notably, training with the ReStore resulted in a significant increase in unassisted maximum gait speeds of 0.07 m s −1 in 36 people with chronic stroke after a brief training of five sessions 122 , which is about a fourth of the dose of non-robotic training regimens, with a median dose of 20 sessions with pooled mean differences of 0.11 m s –1 (ref. 166 ). Training with the Indego device resulted in an average walking speed of 0.37 m s –1 in 32 individuals with SCI who were otherwise non-ambulatory without the device, after 26 visits 161 , which is about half the median dose of body-weight-supported treadmill-walking regimens (50 sessions), which did not increase walking speed 167 . In contrast to the aforementioned devices designed to provide assistance during walking, the Anklebot, which provides isolated training of the paretic ankle joint while seated, led to the transfer of gains from seated training to improvements in walking speed in 29 less-impaired individuals in the chronic phase of stroke 168 .
These findings highlight the potential of robot-assisted interventions in improving clinical outcomes. However, larger trials with control groups are needed to fully understand the generalizability of these results, the practicality of these technologies in the clinic and dose-response relationships over time. Importantly, exoskeletons must show clinically meaningful changes in walking performance in clinical trials. Specifically, RCTs seek to minimize biases in testing, thus increasing the likelihood of revealing robust effects of robotic training compared with conventional approaches 169,170 .
The effects of robotic training in people with stroke 112,113,171,172,173,174,175,176 and other neurologic conditions, such as MS 177,178 and TBI 179 , have been examined in RCTs. In people with chronic stroke, training with the SMA improved walking endurance, daily step count, corticomotor excitability of the paretic rectus femoris 112 , step length and spatial gait symmetry 113 , as compared with a control group who received non-robotic gait training only. Similarly, training with the Lokomat resulted in improvements in gait speed, balance and self-sufficiency 175 . Conversely, training with the Bionic Leg, a powered unilateral knee orthosis, failed to show benefits in gait speed in people with chronic stroke, and showed only modest functional benefits relative to gait training without robotics 172 .
Robotics have thus far only been applied in a subset of people with subacute stroke and substantial gait impairments. Training with the Lokomat 173 and HAL 174 led to a statistically significant increase in functional walking independence in people post-stroke, as well as to tendencies to increased walking speed following training with the treadmill-based Gait Assistance Robot 171 , as compared with gait training without robotics. Although less explored, early stroke rehabilitation during the acute phase or inpatient care may be one of the most relevant applications for exoskeletons. A large number of individuals with stroke are admitted to the hospital, and thus an ideal therapy design at this stage may be most advantageous, minimizing the development of compensations.
Training with the Lokomat also resulted in improvements in walking endurance and speed in people with MS, compared with conventional non-robotic training 178 . Training with the Gait Trainer resulted in improvements in balance; however, this effect was not significantly different compared to control training without robotics 177 . Favourable effects with the Lokomat were also observed in people with TBI, with an improvement in maximum walking speed and step length; however, walking endurance was only improved in non-robotic control training 179 .
Owing to the limited benefit of robot-assisted interventions over conventional gait training thus far 24,25,29,30 , treadmill-based exoskeletons are not currently clinically recommended for gait rehabilitation therapy of people with chronic stroke, incomplete SCI or TBI 180 . Nevertheless, the outcomes of RCTs can inform future clinical-trial designs to improve the quality and staging of the clinical studies with regards to appropriate outcome measures, dose-response effects and control groups for training-effect comparisons 181,182 . The device, training paradigms and patient-inclusion criteria need to be optimized to maximize the benefits of exoskeletons in gait rehabilitation 183 . A change in clinical practice is only justified if new interventions lead to a substantial benefit over existing practice 180 . Therefore, an RCT must be replicated across multiple testing sites to reduce bias and increase generalizability, which is regarded as the gold standard for therapeutic interventions 181 .
The pathway to multicentre RCTs with robotic devices should include four phases 181 . In phase 1, preliminary experiments should be conducted to confirm the safety of the device and its feasibility for clinical use. Clinically relevant outcome metrics, potential training paradigms and participant-inclusion criteria should also be determined at this phase. Once these phase-1 experiments confirm user safety and suggest improvements of clinical outcomes, then more detailed experiments, such as case studies with several participants, can be conducted in phase 2 to further inform training paradigms. Small case studies are more appropriate for substantiating preliminary phase-1 results in clinical settings, but do not require data from more participants than in phase 1. Case studies should include measurements of clinical and biomechanical metrics to enable preliminary explanations for high-level functional changes, such as gait speed. To provide initial insight into how the device compares to conventional therapy without robotics, case studies should involve a preliminary control group that receives similarly structured intervention without the device. In some cases, such as in the chronic phase of stroke, a crossover design can be applied; in this, the participants serve as their own control, and complete interventions with and without the device. Proper device validation in phases 1 and 2 aids in the formulation of the design of an RCT in phase 3 to ultimately enable evidence of intervention validity across multiple testing locations 181 in phase 4. Therefore, if questions regarding intervention dosage, outcome metrics or participant inclusion remain unsolved on completion of phase 2, phases 1 and 2 should be repeated before progressing to phase 3. Similarly, if clinical outcomes are substantially improved but cannot be explained by quantitative biomechanical evaluations, phase 2 must be extended to better understand the human–robot interaction. Once functional outcomes have been shown to improve with the device with respect to the control, and once preliminary biological mechanisms have been identified, an RCT in phase 3 can be performed. An RCT must be sufficiently powered and contain a formal control group representative of usual care, to allow for comparisons of rehabilitation effects. If an RCT shows positive changes in some metrics but remains overall inconclusive, then progression to a multicentre RCT in phase 4 should be halted. Once clinically meaningful average improvements are obtained with the device (compared with the control group), a multicentre RCT can be conducted. Clinical effectiveness from such a study would motivate device implementation in clinical settings.
Only few exoskeleton systems have thus far been tested following this evidence-generation pathway. Although RCTs have shown promising clinical benefits related to speed and functional independence, these effects appear to be specific to the patient population and to the robotic devices (spanning a range of robotic systems, designs, controllers and interactions with diverse patient populations and impairment presentations 184 ). It is important to identify which patient population would benefit the most from the robotic device 185 , rather than assessing a robot’s generalized benefit for all users 184 . Similarly, devices should be developed that can adapt to therapy, community settings and user needs to understand how exoskeletons can best support rehabilitation.
Therefore, clinical trials of neurorehabilitation involving robotics have to adopt strategic staging 181,186 , akin to stepwise and iterative processes employed in the development of drug-based therapies 186 , to minimize premature entry into multicentre RCTs. A comprehensive evaluation of effects of exoskeletons beyond functional outcomes is necessary to identify the underlying mechanisms that pertain to motor recovery versus compensations. However, clinical trials often lack the data required to perform quantitative biomechanical evaluations. Clinical outcomes, such as walking-speed improvements, may be similar in different interventions, but the underlying neural-control strategies may be distinct 112,113 . Robotic interventions can deliver high-intensity and high-repetition practice, which are known drivers of neuroplasticity and which should be considered in clinical trials involving robotics 187 . Understanding neuroplasticity mechanisms can drive neurotechnology design for rehabilitation 188 , considering that common neurorehabilitation practices value motor recovery over compensations. Spatiotemporal measurements from onboard sensors could shed light on the biomechanical mechanisms that lead to functional changes 189,190 ; for example, by mapping neural signals obtained by electroencephalography (EEG) to gait kinematics 191 . In addition, temporal aspects of gait training should be considered. Clinical trials have thus far mainly focused on the rehabilitative potential of exoskeletons; however, the effective frequency and duration of training, and how long benefits may last, remain to be investigated 185 . Also, studies of assistive devices for continuous wear remain limited, but may allow for rehabilitation beyond the clinic and encourage community participation.
Accurate joint-angle estimation has proven invaluable in planning assistance. Most rigid systems use encoders on actuated joints to determine joint angles; however, devices without rigid joints cannot rely on encoders and thus must use other sensors (for example, inertial measurement units; IMUs 192,193 ) to determine joint angles. IMUs are lightweight, inexpensive and easy to integrate into robotic systems, but also particularly sensitive to their physical alignment with biological joints (a challenge that rigid devices do not face). Furthermore, orientation measurements from IMUs suffer from inherent inaccuracies owing to bias (a constant offset compared to the true IMU orientation) and drift (a history-dependent change in orientation), which render measurements unusable within minutes if left uncorrected. Therefore, ensuring consistent alignment without first making precise measurements is difficult, hence IMU-based joint angles can be highly variable depending on placement. Importantly, asking wearers to take precise measurements each time they put on an exoskeleton hinders commercial applications, for which usability is crucial. Misalignments can be corrected by optimization algorithms that automatically estimate the location of the IMU relative to a biological joint, greatly improving joint-angle estimation accuracy 194,195,196,197 . Integrating these algorithms with wearable devices may enable the development of controllers that leverage joint-angle estimates for targeted assistance without requiring rigid joints. Such motion sensing could also be a valuable tool in the evaluation of a wearer’s kinematic performance outside of laboratory settings and could allow for the assessment of interventions at home or in the community. Furthermore, small IMUs worn during walking could inform an algorithm that determines the primary joint (or joints) at which a person experiences a gait deficit, along with the severity of that deficit. A clinician could then recommend a device appropriate for this specific deficit.
Exoskeletons are often controlled by applying actuation profiles as a function of the gait cycle (a standard time-normalized period that stretches from one heel strike to the next). Thus, parallels can be drawn between controllers, biological kinematics and kinetics. Heel-strike events can be assessed via the measurement of the foot switch, by placing an instrumented insole inside the shoe. Although simple in their design, foot switches often have issues related to sizing (the sensor must align well with both the heel and the ball of the foot) and durability (loading well exceeds body weight with every stride). Alternatively, IMUs can be used to detect heel strikes 82,124 . Detection of gait events is easiest with IMUs placed at the ankle, where the impact from a heel strike is most apparent. The cyclical nature of the gait cycle can also be leveraged by identifying measures in the phase plane that remain invariant across walking speeds 198,199 . Devices not targeting the ankle can be equipped with an adaptive oscillator 99,100,105,106,107,108,200 , which takes cyclic measurements of the hip angle to estimate the gait cycle. Instead of measuring the gait cycle, devices can also be designed to actuate in reaction to specific events as they occur 119 . Recent work has used machine-learning techniques to automatically detect the gait cycle using sensors at the hip 201,202 and ankle 203 , adapted to different terrains and walking speeds.
The cyclical nature of walking enables the detection of repeated phases; however, gait initiation, termination, speed changes or turns can happen at any point during the gait cycle and are thus more challenging to detect. Therefore, exoskeletons often rely on sensor input to measure intent of movement and to predict the wearer’s motion before it occurs, to appropriately adjust assistance. However, detecting intent of movement is distinct from activity classification, in which heuristic methods or machine-learning techniques are used to identify activities beyond level-ground walking (such as walk-to-run transitions; or walking on terrains such as ramps or stairs 204,205 ). Similar to detecting the gait phase, the intent of stepping can be detected using IMUs that measure joint angles and angular velocities 206 and that estimate the centre-of-mass position 64 . Other motion-sensing modalities have also been integrated with lower-extremity exoskeletons to detect the intent of movement; for example, surface EMG can be applied to measure muscle activity and to administer proportional assistance at the ankle 35 . Myoelectric control can be further extended by integrating intricacies, such as adaptive gains 137 , and has been shown to be feasible in post-stroke gait 207 across variable speeds 208 . However, surface EMG measures muscle activation rather than muscle motion, which may limit its ability to predict user intention. Alternatively, ultrasound imaging can be applied to sense differences in muscle dynamics for the detection of motor intent 209 . Such real-time estimation of muscle–tendon kinematic behaviour could be incorporated in exoskeleton-control schemes 210 . Although more common in upper-extremity exoskeletons, EEG for intent detection has also been explored in gait-related applications 211 . The NeuroRex was the first lower-extremity exoskeleton to integrate a brain–machine interface into its control loop, detecting a wearer’s motion intention to assist with sit-to-stand 65 and walking 66 .
In functional electrical stimulation (FES), electrical impulses are delivered to a given muscle to generate involuntary contraction and to facilitate movement in paralyzed or weak limbs 212,213,214 . However, such external stimulation saturates muscle activation and can rapidly induce muscle fatigue, which increases the metabolic cost of walking compared with walking with an exoskeleton 215 . However, electrical stimulation can be combined with mechanical assistance. Although more common in upper-limb exoskeletons, electrical stimulation can also be integrated in lower-extremity exoskeletons to create hybrid systems for gait assistance 216 , particularly in people with paraplegia. The Vanderbilt Exoskeleton was the first hybrid system for paraplegic individuals. This hip-and-knee joint-coupled exoskeleton contains a push-button control to stimulate the quadriceps and to generate hip flexion and knee extension 62 . Kinesis, a knee-ankle-foot exoskeleton, similarly combines FES and mechanical assistance to balance the power contribution of the exoskeleton and muscle stimulation. Here, the closed-loop control of FES is based on EMG-estimated muscle fatigue 217 . Such hybrid systems are promising for promoting neuroplasticity because FES interfaces directly with the neuromuscular system and exoskeletons enable high training intensity. Hybrid FES–exoskeleton systems have mainly been explored for paraplegic applications thus far but may also benefit populations with more residual volitional contribution, such as people post-stroke.
Actuator choice for exoskeletons is targeted towards limiting the distal mass and its costly metabolic impact 218 . Accordingly, actuators have been designed to minimize weight and to maximize power. For example, conventional motors can be applied to actuate rigid links and to establish sophisticated interfaces between exoskeletons and the body 104,219,220 . Bowden cables, which can transmit forces from a heavy actuator to lighter-weight distal components, have been applied in both autonomous 117,118,145 and offboard devices 77,79,82,85,115 . Alternatively, McKibben-type pneumatic artificial muscles can distally apply sagittal-plane assistance 34 , with updated versions demonstrating metabolic benefit 67,68,138,207 . Other artificial-muscle technologies have also shown promise for reducing drop foot in people post-stroke 221 . Such soft inflatable actuators have been integrated into research devices for lateral ankle support 222,223 and in commercial devices for recreational knee-injury prevention 224 . As a semi-active extension of a passive exoskeleton 45 , a proof-of-concept electroadhesive clutch has been designed to actively engage or disengage a spring when voltage is applied across a stack of thin electrode sheets 225,226 . These contrast with traditional mechanical clutches, which require a physical latch to engage or disengage a spring, requiring much more elaborate mechanisms. Electrostatic clutches could allow for the design of passive joint-targeting exoskeletons that adapt to changes in speed, movement and the environment.
High-fidelity simulations are an important tool for estimating the metabolic benefit of exoskeleton devices. Empirical techniques, such as HIL optimization, can optimize assistance in response to real-time measurements. In addition, the simulation of forward dynamics can be applied to analytically estimate the impact of exoskeletons, primarily in unimpaired users, but also in rehabilitation 227 . Forward-dynamics simulation can aid in the prototyping of new designs or modes of assistance, and in gaining insight into the biological mechanisms leading to empirical results. For example, exoskeletons have had limited success in lowering the metabolic cost of running; however, a simulation applying ideal torque actuators in seven different configurations to a running model 228 could confirm experimentally observed phenomena, such as a decrease in muscle activation at unassisted joints 115 . A simulation of walking with heavy load suggested, somewhat surprisingly, that hip-abduction assistance could lower the metabolic cost of walking more than (the well-studied) ankle plantarflexion; however, this result remains to be experimentally confirmed 153 .
Machine-learning techniques will allow researchers and clinicians to more efficiently identify people who could benefit from wearable devices. Machine learning can be applied to identify deficits in individuals and to predict the response to robotic interventions; this has been shown in upper-limb exoskeletons and could also be applied to lower-limb devices. For example, in upper-limb rehabilitation, an artificial neural network could predict changes in clinical scores throughout an 80-day exoskeleton-enabled training period in people post-stroke 229 . Similarly, baseline data from individuals with MS have been used to predict changes in clinical measures after 8 weeks of conventional rehabilitation 230 . A combination of movement presentations and demographic data has allowed for the subgrouping of patients to identify deficits in individuals 231,232 and to find characteristic mechanisms that can explain differences between subgroups within a larger clinical population. These data-driven methods can also distinguish between categories of impairments 233 , and automated subgrouping methods can be applied to recruit representative participants for in-depth studies (for example, by using machine learning for patient selection 234 ).
Advances in exoskeleton technology at the system and component levels have contributed to the design of exoskeletons that are ready for clinical integration. Commercial devices are now available for clinical rehabilitation, and Food and Drug Administration (FDA)-approved exoskeletons can return walking ability to individuals who otherwise are unable to walk. Various research-grade exoskeleton devices have contributed to the understanding of the mechanisms by which users can leverage exoskeleton technology. However, clinical and commercial acceptance of exoskeletons remains limited; large-scale RCTs have shown inconclusive results, causing some clinical guidelines to recommend against the use of exoskeletons in gait-training applications for chronic stroke, SCI-i and TBI 180 . Moreover, the vision for recreational exoskeletons to extend walking capacity of unimpaired users remains to be fulfilled, and the driving factors for users to choose exoskeletons remain an important consideration.
Advances in sensing technologies and their integration with wearable devices will help reveal biological mechanisms to enable optimized control. For example, ultrasound imaging has been used with a soft exosuit to reduce the metabolic cost of walking by detecting instantaneous changes in muscle function and by modulating exosuit assistance accordingly 210 . Similar technologies could enable wearable devices to quickly adapt to individual wearers or unknown environments. Small body-worn sensors can measure muscle–tendon forces in real time in vivo 235 ; if implemented in wearable robots, they could offer a metric of user effort and provide insight into how wearable devices can offload stress on soft tissue. Lightweight wearable sensors could be combined with exoskeletons to adapt body-worn devices to a range of activities, environments and wearers, by estimating kinematics during movement, as already demonstrated in the upper extremity with a soft sensing shirt 236 . Indeed, recent work with a joint-targeting autonomous ankle exoskeleton used wearable sensors and a data-driven model to predict the metabolic benefit of a particular control configuration. Using HIL optimization, exoskeleton assistance was adapted as the wearer walked outside the lab 237 . Real-time inverse-dynamics feedback has further been applied to show that healthy adults can accurately target a specified amount of ankle power 238 . Although limited to an instrumented treadmill and not yet suitable for autonomous exoskeletons, similar approaches may increase the understanding of how exoskeletons, which often augment the production of ankle power, interact with the body. Recent work has also used machine-learning techniques to estimate hip moments without requiring an instrumented treadmill 239 .
In addition to sensing modalities, new approaches to actuation and control can be integrated into exoskeletons. Muscle-inspired technologies, such as fibre-based actuators 240 and other compliant actuators 218 , would enable soft actuators with an efficiency similar to biological actuators. Adding machine-learning techniques on top of more conventional control schemes such as adaptive oscillators may allow devices to quickly adapt to changes in walking condition 241 . The availability of more commercial devices will certainly contribute to a better understanding of the physiological impact of exoskeletons. Furthermore, accurate metabolic-cost estimates have to be implemented as real-time input to exoskeleton-control schemes to better prescribe assistance and to maximize individual metabolic-cost reductions. Ultimately, long-term investigations will be required to determine the relation of metabolic-cost reduction to a reduction in injury risk, an increase in wearer performance and an improvement in recreational capacity. These are especially important factors because it is unclear how sensitive individual wearers are to changes in metabolic cost 242 . Additional work may extend beyond metabolic cost to incorporate user preferences to rapidly adapt assistance to particular individuals and walking conditions 243 .
Multicentre RCTs are informative but are time-consuming and resource-consuming, which is not conducive to rapid prototype development 244,245 . Collaborations between clinicians and exoskeleton designers will enable targeted case studies with a small number of selected participants to inform biological mechanisms that warrant larger clinical trials and drive changes in functional outcomes, to enable the design of optimization algorithms for individualized assistance. Understanding disconnects between device function and clinical-trial goals, and quantifying challenges in clinical implementation will be instrumental in directing future studies. Importantly, patients should be included in the design of well-controlled case studies to understand how the devices can improve engagement in the clinical process, for example by following policies established for pharmaceutics 246 .
Rehabilitation studies with exoskeletons typically have the aim of demonstrating clinical efficacy (for example, an increase in walking speed) in a broad patient population, which is often divided into ‘responders’ and ‘non-responders’. A thorough understanding of the biomechanical and neurological mechanisms contributing to clinical outcomes in each subgroup would allow for the grouping of participants before recruitment. For example, machine-learning approaches may be applied to help clinicians prescribe a type of exoskeleton or a particular mode of assistance that will most probably improve walking for an individual user. Industry-wide standards for reproducibility that benchmark device comfort and utility will also give clinicians a clearer understanding of what clinical changes to expect 247,248,249 .
Online optimization methods that can identify optimal assistance profiles in healthy individuals 78,85,250 may also apply to clinical populations. However, HIL techniques typically demand long experiment times, often requiring hours of continuous walking. For widespread application in the clinic, efficient automatic tuning algorithms will be needed that can tailor exoskeleton assistance to a single user.
Using kinematics data from an individual’s prior walking sessions with an exoskeleton may enable exoskeleton-assistance tuning without online optimization. This strategy has been employed for people post-stroke walking with an ankle-assisting wearable robot, where their pre-recorded walking data were used to selectively apply either positive or negative augmentation power 251 . However, to define optimal clinical outcomes, more than a single biomechanical objective is required. Therefore, appropriate clinical objectives that can be measured by devices need to be defined to be able to automatically modulate exoskeleton assistance to an individual patient’s goals. Warm-starting HIL algorithms with baseline data may enable devices to adapt to exoskeleton users as their gait changes across environments or with time. It may also be possible to predict the impact of robotic exoskeleton training before completing a full protocol, although such approaches have been validated only in the upper limb 252 . Ideally, the rehabilitation goals set by patients and clinicians will be achieved by automatic tuning of wearable-device settings. Individualizing assistance by tailoring physical designs to particular wearers through modular systems that can quickly switch from one target joint to another has proven encouraging in an early feasibility study 253 .
In addition to efficient patient selection, the temporal changes in the interaction between an individual and an exoskeleton need to be understood to be able to tailor individual training regimens. Neuromuscular studies provided insight into how individuals adapt to new environments, including the influence of wearable devices on ankle impedance 254 . This knowledge could be integrated in robotic rehabilitation. Studies of upper-limb rehabilitation have shown that it may be possible to distinguish between motor learning and adaptation to a device. Such data would allow for the interpretation of changes in response to training with an exoskeleton to address baseline impairment 255 . Locomotor-adaptation studies using the split-belt treadmill have revealed that people post-stroke showed improvements in gait symmetry after training with error augmentation in the short-term 256 , which can be extended to long-term retention by increasing training 257 and translated to overground environments 258 . Furthermore, learning outcomes may be improved by appropriate intervention scheduling 259 through intermittent exposure and by increasing the variability of training through the introduction of perturbations 260,261 . Challenging the user is also important, and an ‘optimal’ challenge may maximize retention 261 ; for example, increasing propulsion demands using inclined split-belt treadmill training improves gait symmetry post-adaptation more than flat split-belt treadmill training in people post-stroke 262 ; also, high-intensity robot-assisted gait training increases walking speed 263 . In addition to implicit learning pathways, rehabilitation schemes often also incorporate explicit learning through task-specific instructions or biofeedback, which are known to improve learning and rehabilitation outcomes 264,265 . Further investigating these variables in exoskeleton-enabled rehabilitation and long-term exoskeleton use will enable the design and development of training regimes that promote neuromotor recovery.
Interaction between clinicians and patients is often limited, with supervised therapy in the United States typically ending 6 months after a stroke, despite evidence of the benefits of long-term exercise 266,267,268 . The American Physical Therapy Association, an advocate of telehealth practices, recognizes the potential of expanded access to physical-therapy services 269 . Telehealth practices have been widely used in response to the COVID-19 pandemic and may continue to be applied. Determining how gait training is administered and monitored outside of the laboratory and the clinic becomes increasingly important 270 . Exoskeletons have the potential to be remote gait-training tools that supplement in-person therapy.
Devices designed for remote use could include real-time biometric monitoring of the wearer’s response; for example, skin-adhering flexible sensors can measure vital signs 271 . In addition to monitoring wearer safety, such sensor systems may be especially valuable in home or community environments for device control; that is, to modulate assistance and to encourage more user effort; or for user feedback, for example by providing a summary of exertion during walking. Integrating wearable sensors 272 into wearable devices will enable more individualized and robust exoskeleton control, and improve remote-activity monitoring and performance reporting.
Ensuring user safety is a key exoskeleton-design consideration for unsupervised or remotely supervised community-based or home-based gait training. Unlike upper-extremity training, gait training inherently incurs a fall risk. Importantly, for gait training with a powered exoskeleton, wearer instability must be limited in the case of device failure. The unsupervised use of exoskeletons requires the design of streamlined devices that can be donned and operated by the wearer. Especially at the ankle, designers may wish to introduce additional active degrees of freedom to promote natural joint motion without sacrificing stability 273 . Improvements in adaptability and comfort will make future exoskeletons not only tools for gait training, but also all-day wear devices that increase the performance of everyday walking. To determine the fit and comfort during extended wear, metrics are needed that quantify device component fit 274 , and techniques are required to quantify the pressure exerted by exoskeleton attachments 275 . In addition, the human–machine interface needs to be closely monitored, in particular for users with reduced sensation in their impaired lower extremities.
Advances in exoskeleton technology will allow the integration of wearable devices in the daily lives of patients, clinicians and recreational users. Pioneering work in exoskeleton technology revealed how exoskeletons interact with (and modify) the basic physiological mechanisms of walking. This physiological understanding has made it possible for wearable robotic exoskeletons to reach clinical use. We believe that new component technologies will underpin the next decade of wearable robotics, and envision that exoskeletons will become an integral part of daily life.
We thank L. Schumm and D. Orzel for help with the illustrations. This work was supported by the National Institutes of Health under award numbers BRG R01HD088619 and R01AG067394, and by the American Heart Association grant AHA 18TPA34170171. This work is based on studies supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE1144152, and by the National Science Foundation under Grant No. CMMI-1925085.